Understanding Kidney Protein Loss: Causes and Impact
Intro
The kidneys play a vital role in filtering waste from the blood, maintaining balance in body fluids, and regulating various electrolytes. However, when protein loss occurs in the kidneys, it can signify underlying issues that demand attention. Proteinuria, which is the clinical term for excess protein in the urine, can stem from numerous factors and may have significant consequences on overall health. Understanding the dynamics of protein loss is crucial for healthcare professionals and anyone interested in human physiology. It isn’t just about the kidneys; it encompasses a wider context of body health.
The importance of grasping the nuances behind protein loss cannot be overstated. The consequences can range from mild to severe, depending on the underlying causes. In this article, we will break down the complexities of protein loss in the kidneys, exploring various aspects such as its physiological underpinnings, associated disorders, diagnostic approaches, and potential treatments.
Key Concepts
Understanding certain concepts is essential for delving into the topic of protein loss in kidneys. Here, we clarify some primary terms and related theories.
Definition of Primary Terms
- Proteinuria: This is characterized by the presence of an abnormal amount of protein in the urine. Normal urine usually contains little to no protein, so its detection can be alarming.
- Glomeruli: These are tiny filters in the kidneys that remove waste and excess substances from the blood. Damage to these filters is a common cause of protein loss.
- Nephrotic Syndrome: A group of symptoms indicating significant protein loss due to kidney dysfunction. This may include swelling, high cholesterol, and increased triglycerides.
Related Concepts and Theories
The discussion of protein loss often intersects with various other medical concepts. These can provide insight into how proteinuria fits within broader health frameworks:
- Inflammation and Immunity: The immune response may contribute to kidney damage, leading to protein loss. For example, certain autoimmune diseases can affect kidney function directly.
- Hypertension: High blood pressure can damage the glomeruli, facilitating protein loss. The relationship between kidney health and blood pressure regulation cannot be ignored.
- Diabetes: Diabetic nephropathy is a common complication in diabetes, where kidney damage results in increased protein excretion.
"Understanding the intricate links between kidney function and systemic diseases is key to addressing protein loss effectively."
Future Directions
While much has been uncovered regarding kidney health and proteinuria, several gaps remain in our understanding. Further studies are crucial for advancing this field.
Gaps Identified in Current Research
- Longitudinal Studies: There is a lack of long-term studies assessing the effects of protein loss on different demographic groups. More of these studies could clarify how age, gender, or ethnicity interact with kidney health.
- Molecular Mechanisms: While we have basic knowledge about the causes of proteinuria, detailed understanding of the molecular pathways involved is still very limited.
Suggestions for Further Studies
Researchers could investigate areas such as:
- The impact of lifestyle changes on protein loss and kidney health. For instance, examining dietary modifications and their effects would be valuable.
- Advanced diagnostic methods that could improve early detection of kidney disorders associated with proteinuria.
Foreword to Kidney Function
The role of the kidneys goes well beyond mere urine production. Often hailed as nature’s purifiers, the kidneys are crucial players in maintaining homeostasis—balancing fluids, electrolytes, and electrolytes for optimal bodily function. Understanding kidney function provides essential context for discussing protein loss, which can have profound implications on health.
By grasping how the kidneys work, one can better appreciate the mechanisms that lead to proteinuria. This foundation sets the stage for exploring the various kidney disorders associated with protein loss, their diagnostic approaches, and the potential treatments available. In short, knowing the ropes of kidney function illuminates the path to better health and well-being, especially as it relates to conditions that might arise or worsen due to protein loss.
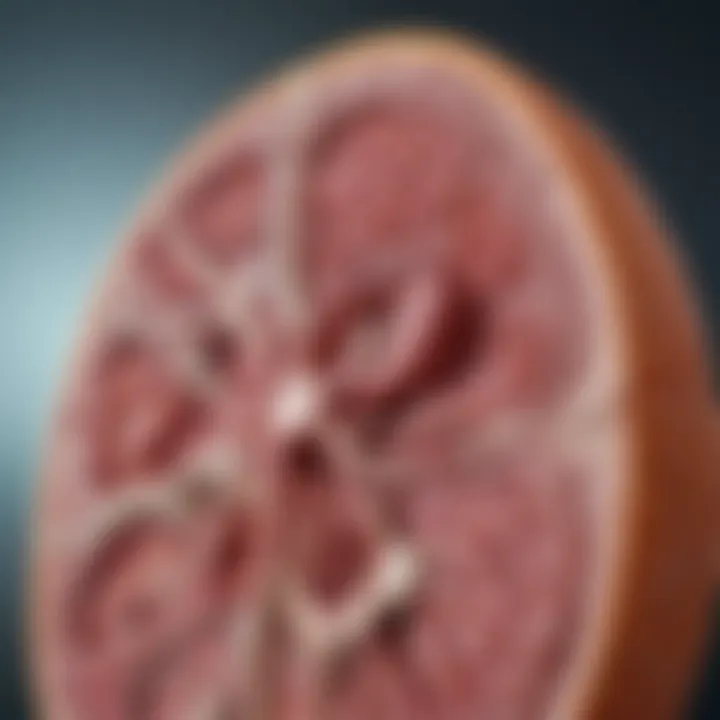
The Role of Kidneys in Homeostasis
Kidneys aren’t just bean-shaped organs tucked away in the lower back; they serve as vital regulators of our internal environment. They maintain the balance of essential substances, including water, electrolytes, and waste products. This delicate equilibrium is crucial for sustaining a stable internal environment, also known as homeostasis.
Filtration is a key process here. Blood gets filtered through millions of tiny structures called nephrons, where valuable substances like proteins and glucose are reabsorbed into the bloodstream, while waste materials are sent to the bladder for excretion. Essentially, kidneys help the body decide what stays and what goes. If they falter, we could find ourselves in hot water, facing conditions that may lead to renal failure or systemic health issues.
"Healthy kidneys do not just filter blood; they maintain the vital balance requiring precision and coordination that we often take for granted."
Understanding Glomerular Filtration
Glomerular filtration is the first step in urine production and serves as a litmus test for kidney health. The glomeruli—tiny capillary loops in the nephron—are responsible for filtering blood plasma based on size and charge. It’s like a highly selective sieve. Small molecules such as water, ions, and glucose pass through while larger ones, particularly proteins, should ideally remain in circulation.
A number called the glomerular filtration rate (GFR) quantifies this filtering ability, providing a snapshot of kidney performance. Healthy kidneys showcase a GFR that allows for efficient waste removal while retaining necessary proteins and blood cells. Any dip in this filtration rate can signal issues ranging from dehydration to kidney disease, initiating a cascade of health ramifications, including protein loss.
In essence, understanding glomerular filtration is imperative for anyone delving into the complexities of kidney-related disorders. It lays the groundwork for diagnosing and managing conditions like proteinuria, providing insights that are essential for healthcare professionals and informed patients alike.
Protein Loss: Definition and Mechanism
When we talk about protein loss in the kidneys, it’s not just a medical term tossed around in clinics; this concept holds significance in both patient care and broader health implications. The kidneys play a crucial role in filtering waste, and understanding how and why protein loss occurs can unveil essential insights into the state of renal health. Protein, primarily albumin, can be a marker for more complex underlying health issues. If we can grasp this topic, we can better approach diagnosis, treatment, and even preventive measures.
What is Proteinuria?
Proteinuria refers to the presence of abnormal amounts of protein in the urine, a condition that can indicate an underlying issue with the kidneys. In a healthy system, the kidneys efficiently filter blood, retaining essential proteins while allowing waste to exit through urine. However, when there’s a disruption, proteins that should remain in the bloodstream sneak into the urine. It’s not just the quantity of protein that matters; the type and duration of proteinuria are equally significant. Transient proteinuria might arise due to temporary causes such as exercise or fever, while persistent proteinuria often signals chronic renal problems or systemic diseases. Recognizing and diagnosing this condition early can be key to managing potential kidney damage.
Quantifying protein levels plays an important role. The urine protein-to-creatinine ratio can distinguish between the types of proteinuria. What can sometimes go unnoticed is that proteinuria isn't just a single symptom; it can serve as an indicator of broader issues, such as diabetes or hypertension, potentially altering treatment trajectories.
"The detection of proteinuria is often a silent alarm in the body. Addressing it promptly can prevent more severe health ramifications."
Mechanisms of Protein Loss in Renal Pathology
To get to the roots of protein loss, it’s essential to dissect the mechanisms at play within renal pathology. There are several pathways that lead to proteinuria, often categorized based on where in the nephron—the functional unit of the kidney—these aberrations occur.
- Glomerular Damage: The glomeruli filter blood in the kidneys. Damage to these structures can lead to excessive protein leakage. Conditions like glomerulonephritis or the nephrotic syndrome showcase this mechanism. Here, the integrity of the filtration barrier is compromised, allowing proteins to slip through.
- Tubular Dysfunction: The renal tubules are responsible for reabsorbing proteins back into the bloodstream. When they fail to function optimally, protein loss ramps up. Interstitial nephritis often exemplifies such issues, where damaged tubules cannot recover proteins effectively.
- Overproduction: It’s not only about what the kidneys can’t handle but also what the body creates. In certain diseases, such as multiple myeloma, excessive production of light chains can overwhelm the filtering capacity of the kidneys.
- Increased Vascular Permeability: Inflammatory conditions can increase blood vessel permeability, causing proteins to leak into the urine.
Each of these mechanisms emphasizes how multifaceted kidney issues are and illustrates the importance of identifying the precise cause behind protein loss. Coping with renal pathology isn’t merely about treating the symptom; it’s about addressing the underlying mechanisms to provide effective management.
In summary, defining protein loss and understanding its mechanisms provides a window into the complexities of kidney function and disorders. This understanding is vital for students, researchers, educators, and professionals, as it lays the groundwork for informed discussions around diagnosis and potential interventions.
Types of Protein Loss
Understanding the different types of protein loss is crucial for grasping the overall implications of kidney dysfunction. Each category of proteinuria—whether it’s transient or persistent—presents unique challenges and requires specific diagnostic considerations. Recognizing these differences can greatly affect the management strategies employed, ultimately impacting long-term patient outcomes.
Transient vs. Persistent Proteinuria
Transient proteinuria often occurs due to various factors such as intense exercise, stress, or dehydration. This temporary increase in protein levels is typically benign and resolves after addressing the underlying cause. It's a classic case of ‘the hiccup that passes’, where the body responds to external stimuli. However, while it may not raise immediate alarm bells, it's essential for healthcare practitioners to monitor these instances, especially when they coincide with other symptoms.
On the other hand, persistent proteinuria is a red flag indicating chronic kidney disease or other underlying renal problems. Statistics estimate that anywhere from 5% to 25% of adults exhibit persistent proteinuria in their lifetime, underscoring its significance. When protein is continually lost, it signals that something is amiss in the renal system. The patient might not feel any symptoms initially, making awareness even more critical. The consequences of ignoring this condition can lead to worsening kidney function, high blood pressure, or even heart problems, which can be difficult to untangle later.
Nephrotic Syndrome and Its Characteristics
Nephrotic syndrome is a specific and serious form of protein loss characterized by a drastic increase in protein in urine, hypoproteinemia, edema, and hyperlipidemia. This syndrome often emerges from glomerular injury, where the kidney’s filtration units fail to hold onto proteins. The term 'nephrotic' derives from 'nephros,' meaning kidney in Greek, while 'syndrome' implies a group of symptoms that occur together.
Here’s the kicker—nephrotic syndrome occurs in both children and adults but for different reasons. In kids, it’s often idiopathic, meaning the cause is unknown. Meanwhile, in adults, it’s usually related to conditions such as diabetic nephropathy or minimal change disease. Not just a textbook concept, nephrotic syndrome can drastically alter a patient’s quality of life due to severe swelling and increased susceptibility to infections, making timely diagnosis and intervention essential.
Effects of Other Kidney Disorders
Other kidney disorders can also lead to protein loss, each with a unique mechanism contributing to this condition. For example, diabetic kidney disease stems from long-term uncontrolled blood sugar levels, resulting in damage to glomeruli. It’s a snowball effect; once the filtration barriers are compromised, proteins begin to leak into the urine.
Furthermore, chronic glomerulonephritis, caused by inflammation of the glomeruli, can persist for years and is often difficult to diagnose early. This leads to a slow accumulation of damage, resulting in nephron loss and subsequent proteinuria.
"Understanding these underlying conditions is paramount for clinicians and patients alike, as it aids in timely intervention and treatment to prevent progression to more severe kidney ailments."
Other kidney ailments, like polycystic kidney disease, also present a complicated web of symptoms and repercussions. The presence of proteinuria serves as an essential indicator that necessitates comprehensive investigations to determine the right course of action for management.
In summary, the classification of protein loss plays a pivotal role in understanding kidney health. Both transient and persistent forms carry significant implications for patient care, while specific disorders like nephrotic syndrome bring additional complexities to the forefront. Recognizing and diagnosing these types of protein loss not only aids in clinical assessments but also lays the groundwork for tailored treatment plans.
Causes of Protein Loss in Kidneys
Understanding the causes of protein loss in the kidneys is of utmost importance, as it lays the groundwork for diagnosing and managing diseases that can potentially lead to significant health complications. When kidney function falters, the consequences can ripple throughout the body, affecting everything from fluid balance to immune response. By recognizing the specific underlying factors contributing to proteinuria, healthcare providers can tailor interventions more effectively and hopefully mitigate further damage to renal structures.
Diabetes and Its Impact on Kidney Health
Diabetes is a leading cause of kidney disease, particularly because of its stressful impact on the glomeruli—the tiny filtering units within the kidneys. Over time, elevated blood sugar levels can lead to diabetic nephropathy, a condition where damage occurs to the delicate blood vessels delivering oxygen and nutrients to kidney tissues. As the kidneys struggle, they start allowing larger molecules, like proteins, to escape into the urine.
The early signs often go unnoticed, making regular check-ups essential for individuals with diabetes. They might not experience noticeable symptoms until significant damage has already occurred. Control of blood sugar levels is critical; when well managed, the risk of kidney problems decreases substantially. Hence, a diabetic patient would benefit from closer monitoring and intervention strategies that emphasize both glucose control and renal health.
Hypertension and Renal Damage
High blood pressure, or hypertension, can wreak havoc on the kidneys. The increased pressure in blood vessels can lead to thickening and hardening of vessel walls, impeding adequate blood flow to the kidneys. Over time, this can cause glomerular injury. When the glomeruli are damaged, their ability to filter blood effectively is compromised, leading to the spillage of proteins into urine.
For most people, managing blood pressure through lifestyle changes such as maintaining a healthy weight and eating a balanced diet can make a significant difference. In some cases, medication may be necessary. The interplay between hypertension and kidney health highlights the need to monitor both closely in patients suffering from either condition.
Glomerulonephritis and Autoimmune Disorders
Glomerulonephritis is an inflammation of the glomeruli, which may arise from various autoimmune disorders such as lupus. In these scenarios, the body's immune system mistakenly targets the kidneys, initiating a cascade of damage that leads to proteinuria. The inflammation causes the glomeruli to become permeable, allowing proteins to leak into the urinary system.
Patients with autoimmune conditions often experience signs and symptoms that may differ from classic kidney disease presentations. Hence, awareness and prompt diagnosis are paramount. Targeting the underlying autoimmune disorder through immunosuppressive therapies can often help restore kidney function and reduce protein loss.
Infectious Causes of Proteinuria
Infections can also lead to temporary or chronic protein loss in the kidneys. Conditions such as urinary tract infections, pyelonephritis (a kidney infection), or even systemic infections can strain kidney function, prompting them to leak protein. Bacterial infections can lead to inflammation and damage to the kidney’s filtering capacity, while viral infections like HIV can initiate changes in kidney tissue that result in proteinuria.
Prompt treatment of infections is crucial to alleviate their impact on the kidneys. Antimicrobial therapies are often necessary and can significantly improve kidney function when applied early. Patients should be advised to seek medical attention promptly if they experience symptoms related to infections, as early intervention can obviate the progression of kidney damage.
"Being proactive about kidney health means recognizing the signs of underlying diseases that can lead to protein loss, including diabetes and hypertension, is vital in preventing severe complications."
Diagnosis of Protein Loss
Diagnosing protein loss through the kidneys is a crucial process for both understanding the underlying issues and developing tailored treatment options. Proteinuria can be a symptom of various kidney disorders, and identifying its presence is the first step towards addressing these health concerns effectively. The importance of accurate diagnosis goes beyond the name of the condition; it can significantly influence the patient's overall health trajectory and lifestyle choices.
The diagnostic process involves not just the observation of symptoms but a meticulous approach that incorporates clinical assessments, laboratory tests, and imaging techniques. Each element plays a vital role in forming a holistic view of the patient’s condition, enabling healthcare professionals to recognize patterns, identify abnormalities, and recommend pertinent interventions.
"An early diagnosis can be the difference between a manageable condition and irreversible damage to kidney function."
Clinical Assessment and History Taking
In any medical consultation, history taking is often where the detective work begins. In cases of suspected protein loss, a thorough clinical assessment serves as a linchpin in the overall diagnosis. Physicians typically initiate this process with a detailed interview that covers the patient's medical history, family history, and any pre-existing conditions that may contribute to renal issues. Questions often focus on urine color, volume, and frequency, as well as any accompanying symptoms like swelling or fatigue.
From there, a physical examination offers further clues. Notable indicators might include protein levels in the urine, continual weight fluctuation, or unusual swelling in the extremities. This initial engagement sets the stage for what’s next—diving deeper into laboratory tests and imaging, which can provide a clearer picture of the underlying causes.
Laboratory Tests and Procedures
Laboratory analysis is the meat and potatoes of diagnosing proteinuria. The first step usually involves a urinalysis, where a sample of urine is assessed for proteins. A dipstick test can reveal protein concentrations and may indicate the presence of certain diseases. If results suggest an abnormal level of protein, a 24-hour urine collection may be ordered to measure the total daily protein excretion. This helps determine whether the protein loss is transient or persistent.
In addition to urinalysis, blood tests are integral for evaluating kidney function. For instance, tests measuring creatinine levels can offer insight into how well the kidneys filter waste. Abnormal results can indicate more severe underlying conditions that necessitate further investigation.
Imaging Techniques in Diagnosis
Although laboratory tests are essential, imaging techniques add another layer of information to the diagnosis. Ultrasound is a common, non-invasive method that helps visualize the kidneys' structure. It can detect abnormalities such as kidney cysts, obstructions, or other structural changes.
Other imaging techniques, like CT scans or MRIs, might be employed depending on the complexity of the case. These polythetic approaches allow healthcare providers to form a comprehensive picture of kidney health. They assist in deciding the next appropriate steps toward diagnosis and treatment. Understanding how these diagnostic tools interact provides valuable context to the patient's situation and can enhance the overall effectiveness of the management plan.
Combined, these strategies under the umbrella of diagnosis inform every stake in the management of protein loss in the kidneys, setting the foundation for subsequent steps in treatment and care.
Clinical Implications of Protein Loss
The topic of clinical implications regarding protein loss in the kidneys resonates far beyond mere medical nomenclature. It affects real individuals, their families, and the structure of healthcare systems. When we talk about protein loss, we're dealing with complications that, if left unchecked, could alter the very fabric of a patient’s life. Recognizing these implications is crucial for both patients and healthcare providers, allowing for timely interventions and improved outcomes.
Impact on Patient Health and Quality of Life
Proteinuria, or the presence of excess protein in urine, may seem like a technical detail in the larger picture of kidney health, but its effects permeate many layers of a patient’s existence. A patient coping with protein loss is not only facing a potential decline in kidney function but is also juggling a host of physical and psychological challenges.
One of the most immediate consequences of protein loss is its impact on the body's ability to maintain fluid balance. When proteins leak into the urine, it can lead to a condition known as edema, where excess fluid accumulates in tissues, resulting in swelling—usually noticeable in the legs and abdomen. This can hinder mobility and cause discomfort. Moreover, the resulting fatigue and overall malaise can negatively skew a patient's perception of well-being.
"The presence of protein in urine is not merely an isolated finding; it's a signal of something more profound impacting the patient’s health and daily function.”
The psychological burden can be significant as well. Anxiety related to health outcomes, uncertainty about the future, and the need for ongoing monitoring drive many patients into a state of hyper-vigilance regarding their health. It can become a cycle that reduces quality of life, amplifying issues like depression or chronic stress.
To illustrate, consider a patient diagnosed with nephrotic syndrome—a severe type of protein loss. This individual might find themselves in and out of doctors’ offices, undergoing various tests, managing multiple medications, and constantly adjusting their lifestyle. Each aspect requires energy and resilience, and the cumulative effect can feel overwhelming.
Progression to Chronic Kidney Disease
One of the most alarming clinical implications of protein loss is its potential to escalate into chronic kidney disease (CKD). When the kidneys endure prolonged proteinuria, structural damage can occur, leading from minor dysfunction to significant impairments in filtration capacity. Essentially, the kidneys become less efficient at removing waste and excess fluid from the body, setting the stage for CKD—this isn't just a technical milestone but a life-altering transition.
With CKD, the patient's health prospects can dwindle. The body can become more susceptible to ailments, requiring strict dietary regimens and perhaps even dialysis or transplant in advanced stages. The pathway from proteinuria to CKD is not a straightforward journey—various factors influence this trajectory, including age, existing comorbidities, and lifestyle choices.
Furthermore, this progression underscores an essential aspect of patient education—that proactive management of kidney health, including regular follow-ups, can halt or slow the trajectory of disease progression. Understanding this connection prompts both patients and providers to prioritize early detection and effective management strategies.
In light of these dynamics, it follows that addressing protein loss through vigilant medical care is paramount. It’s more than just preventing a number from climbing on a lab report; it’s about securing a more stable, healthier future for those affected.
Treatment Options for Protein Loss

Understanding treatment options for protein loss in the kidneys is essential due to the variety of factors that contribute to proteinuria. Treatment strategies can have significant benefits for patients by addressing the underlying causes, reducing protein loss, and improving overall kidney function. It’s critical for health professionals to tailor these options to the individual’s unique circumstances, while also considering potential side effects and interactions with existing medications.
Medications and Management Strategies
When it comes to medications to manage protein loss, various classes are available, each with its own mechanism of action. Angiotensin-converting enzyme (ACE) inhibitors are frequently prescribed to patients with underlying conditions such as hypertension or diabetes. These medications work by relaxing blood vessels, thus reducing the pressure within the kidneys and helping to decrease proteinuria. Angiotensin receptor blockers (ARBs) offer similar benefits and may be more suitable for patients who experience side effects from ACE inhibitors.
"Addressing protein loss in nephrotic syndrome often requires a multifaceted approach involving both medication and lifestyle modifications."
Medication can also include diuretics, which help to eliminate excess fluid from the body, albeit it is important to monitor kidney function closely while using them. Another class, statins, is sometimes used when patients present with dyslipidemia, as they can aid in lowering cholesterol, an important factor in kidney health.
Aside from pharmacological treatment, healthcare professionals often emphasize regular monitoring of renal function and protein levels. Follow-up visits may involve measuring serum creatinine and urine protein levels, which can inform adjustments in treatment plans. Additionally, some patients may benefit from immunosuppressive therapies in cases of autoimmune disease, with drugs such as corticosteroids being considered based on the patient's condition.
Dietary Interventions and Lifestyle Changes
Diet plays a pivotal role in managing protein loss. First and foremost, reducing sodium intake can help control blood pressure and lessen strain on the kidneys. Foods high in sodium, such as processed snacks, deli meats, and canned goods, should be limited. Instead, patients are encouraged to consume fresh fruits and vegetables, low-fat dairy, and lean proteins.
Another important dietary approach is moderating protein intake. This does not mean eliminating protein entirely but rather ensuring it constitutes a balanced part of the diet. This is particularly relevant for those with chronic kidney disease, as excessive protein can exacerbate the condition.
In addition to diet, lifestyle changes can complement treatment options. Regular physical activity can help manage weight and improve overall cardiovascular health, which indirectly supports kidney function. Moreover, learning effective stress management techniques may contribute to better health outcomes. Stress can lead to elevated blood pressure and potentially worsen kidney conditions.
Lastly, cessation of smoking and moderation of alcohol can have profound impacts on kidney health. Being proactive about these changes can vastly improve the quality of life for individuals dealing with protein loss due to kidney issues.
Preventive Measures for Kidney Health
Preventive measures play a crucial role in maintaining kidney health and mitigating the impacts of protein loss. The kidneys are often referred to as silent workhorses of the body, performing vital functions without much notice until something goes awry. As we delve into this critical area, it becomes clear that proactive steps can make significant differences in kidney function and overall well-being.
Regular Health Check-Ups
Regular health check-ups serve as the cornerstone of effective kidney health management. These assessments help identify potential issues before they develop into serious conditions. Think of it as catching a small leak in a roof before it leads to water damage in your home. Through periodic evaluations, healthcare professionals can monitor kidney function, assess for any early signs of proteinuria, and detect risk factors that might contribute to renal complications.
During these check-ups, doctors typically request a range of tests, including blood and urine analyses. Blood tests can reveal levels of creatinine and urea, while urinalysis can check for abnormal protein levels. Based on these findings, physicians can recommend further evaluations or lifestyle changes.
Moreover, fostering a habit of regular check-ups encourages patients to take ownership of their health. It shifts the focus from reaction to prevention, enabling individuals to make informed choices about diet, exercise, and other lifestyle factors that can bolster kidney function.
Importance of Blood Pressure and Sugar Control
Managing blood pressure and blood sugar levels is essential to safeguard kidney health. High blood pressure and uncontrolled diabetes are among the leading culprits behind kidney damage. When these conditions are left unchecked, they can cause significant strain on the kidneys, leading to conditions such as nephropathy.
Blood Pressure Stability:
- Keeping blood pressure within the recommended range (around 120/80 mmHg) reduces the risk of damage to the blood vessels within the kidneys.
- Medications, dietary changes, and regular exercise can be pivotal in achieving and maintaining optimal blood pressure.
Sugar Control:
- Maintaining blood sugar levels is equally important, especially for diabetics. Elevated glucose levels can damage the nephrons, the kidney’s filtering units.
- Monitoring blood sugar through diet, medications like insulin, and regular testing plays a crucial role in kidney protection.
A wise saying goes, "An ounce of prevention is worth a pound of cure." This notion holds particularly true when considering kidney health. By prioritizing regular health assessments and managing blood pressure along with sugar levels, patients embark upon a path towards healthier kidneys, one that could potentially steer clear of myriad complications associated with protein loss.
"The kidneys may be small, but their impact on overall health is colossal."
Future Directions in Research
As we delve into the nuances of protein loss in the kidneys, it becomes clear that understanding its implications is not just a matter of clinical concern but also a vast field ripe for research exploration. The landscape of renal pathology is constantly evolving, and so are the approaches to diagnosis and therapy. Innovative research initiatives are essential for unraveling the complexities surrounding proteinuria and its associated disorders, particularly as we aim to enhance patient outcomes and inform preventative strategies.
Innovative Diagnostic Techniques
The future of diagnosing protein loss hinges greatly on the development of innovative technqiues. Traditional methods like urine dipstick tests or 24-hour protein collections have served their purpose but come with limitations, including potential inaccuracies and patient compliance issues.
Emerging diagnostic techniques could significantly change how we approach detection and monitoring of proteinuria. For instance, mass spectrometry is gaining traction for its ability to provide a detailed proteomic profile of urine samples. This could facilitate earlier and more precise identification of kidney dysfunction.
- Nanotechnology is also stepping into the ring. Its applications in biosensors could lead to the creation of real-time, wearable devices that monitor protein levels continuously. This approach not only improves patient engagement but also enhances the specificity of monitoring, allowing for timely intervention when levels spike unexpectedly.
- Proteomics represents another exciting frontier, offering insights into the molecular underpinnings of kidney diseases. It not only holds the potential for identifying novel biomarkers but also paves the way for personalized treatment plans, catering to the unique needs of each patient.
The advancement in these diagnostic techniques is promising. As researchers pursue these avenues, a nuanced approach that integrates technology with patient-centered care will likely emerge, making a tangible difference in clinical practice.
Emerging Therapies and Treatment Protocols
As we look to tomorrow, it’s vital to examine not just how we diagnose protein loss but also how we manage it. Effective treatment protocols are evolving, influenced by ongoing research and a better understanding of the underlying mechanisms driving renal dysfunction.
Current options like ACE inhibitors and angiotensin receptor blockers are foundational in managing proteinuria, particularly in conditions like diabetes and hypertension. However, ongoing studies are exploring more cutting-edge therapies:
- Biologic agents, such as monoclonal antibodies, are being investigated for their efficacy in targeting specific pathways involved in kidney injury. This trend might be a game-changer for individuals with nephrotic syndrome or other proteinuric disorders.
- Stem cell therapy remains at the forefront of experimental treatments. Early-phase trials show potential in regenerating damaged kidney tissue and reversing protein loss. If successful, this approach could alter not only prognosis but also the management of chronic kidney disease.
- Comprehensive lifestyle interventions are also gaining attention. Rather than relying solely on pharmaceuticals, the integration of dietary modifications, exercise regimens, and stress management could provide a holistic treatment strategy.
With advancements in understanding how proteinuria affects overall health, therapies are shifting towards a more integrated framework that addresses both the symptoms and root causes.



